Abstract

Background: The incidence of lymphoma concurrently involving the central nervous system (CNS) and systemic organs is very rare. Data regarding this clinical setting are based on case reports and relatively small retrospective series, precluding the establishment of solid recommendation regarding prognosis and treatment.
Objectives: The current retrospective multi-center study investigated the characteristics, treatment protocols and outcome of patients with B cell non-Hodgkin lymphoma (B-NHL), diagnosed with concomitant systemic and CNS involvement, between the years 2004 to 2017.
Results: All consecutive patients with B- NHL, presenting with concomitant systemic and CNS involvement at diagnosis were reviewed. Thirty five patients were included (24 male; 11 females). Median age at diagnosis was 59 years (34-86). Histological subtype was diffuse large B-cell lymphoma in almost all patients (n=34; 97%). The International prognostic index was greater than 2 in 70% of the patients (n=24). The median number of extra nodal sites was 1 (range: 0-4), with bone being the most common extra nodal site (n=14).Concurrent indolent and aggressive lymphoma were reported in 2 out of 30 patients for which these data were available (6.7%). Twenty two patients had paranchymal involvement (63%). Eight patients had meningeal involvement per imaging (23%) and 4 had spinal disease. Cerebrospinal fluid (CSF) involvement, defined by a positive CSF cytology or immunophenotyping, was detected in 59% (13/22 patients).
The most common induction chemotherapy was anthracycline-based (RCHOP / RCHOP like regimen) in combination with high-dose methotrexate (MTX), with or without cytarabine (23 of 35 patients, 66%). Seven patients were ineligible for intensive chemotherapy due to poor performance status. Overall, 14 patients died from the disease (40%). Six of them during induction and 8 due to relapsed/refractory disease. 2 patients died from other causes.
Overall response rate following induction treatment was 80%, including 60% complete remissions (CRs) and 20% partial remissions (PRs). Most patients achieved CNS and systemic CR (evaluated by nervous system MRI/CT and PET/CT).
14 patients were treated with high dose chemotherapy followed by autologous stem cell transplantation (ASCT) (12 in CR and 2 in PR). ASCT did not improve depth of response in any of the patients transplanted in less than CR.
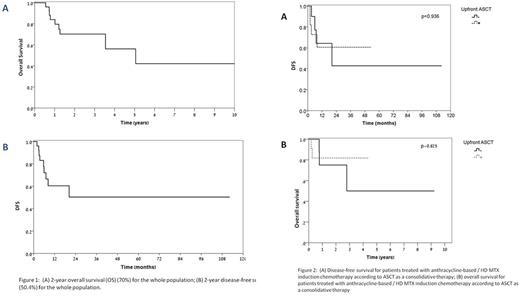
Nine patients (33.3%) relapsed within less than 2 years from diagnosis. Disease-free survival (DFS) and overall survival (OS) of the entire cohort were 50.4% and 70.2%, respectively (Figure 1), similar to patients receiving anthracycline-based / high-dose MTX regimen (47.8% and 79.2% respectively). ASCT did not improve the outcome of patients treated with anthracycline-based / high-dose MTX chemotherapy (figure 2). Paravertebral mass (HR=14.8, p=0.002) rather than brain disease (parenchyma, intraventricular or both), meningeal or cranial nerve involvement and an increased LDH level (HRfor100unit=1.11, p=0.006) were found to be associated with shorter OS.
Restricted analysis, including patients receiving anthracycline-based / high-dose MTX regimen only , found paravertebral mass (HR=38.265, p=0.011) and meningeal disease (HR=10.463, p=0.059) to be associated with an increased risk of relapse. Of note, brain involvement (HR=0.08, p=0.036) was associated with a decrease risk of relapse.
Conclusion: Combination therapy with RCHOP-HD MTX provides encouraging outcome in DLBCL patients presenting with systemic and CNS disease, with half remain free of disease at 2 years post diagnosis. Patients presenting with brain involvement had better survival than patients diagnosed with paravertebral involvement. Our study did not demonstrate clear survival benefit for patients undergoing ASCT, and given the relatively good outcome of our cohort, the benefit of ASCT in this group of patients needs to be further validated in prospective studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal